Menopausal Brain Fog: The Role of Starved Estrogen Receptors in a Woman’s Brain
Introduction
Menopausal brain fog is a real and frustrating phenomenon affecting millions of women worldwide. As estrogen levels drop during menopause, starved estrogen receptors in the brain may lead to cognitive symptoms such as memory lapses, confusion, and slower thinking (Mosconi et al., 2017).
Understanding the connection between estrogen and brain health is essential for supporting women during midlife transitions. This article explores how declining estrogen and receptor starvation impact cognitive performance and offers natural, science-backed solutions to improve brain clarity during menopause.
Understanding Menopausal Brain Fog
Brain fog during menopause refers to a group of cognitive symptoms that typically emerge during perimenopause and postmenopause. Common signs include:- Forgetfulness
- Reduced concentration
- Difficulty multitasking
- Slower mental processing
These symptoms may come and go but can significantly affect daily functioning and quality of life (Weber et al., 2013). Menopausal brain fog is closely linked to the hormonal changes women undergo—particularly the decline in circulating estrogen.
Estrogen and Brain Health
Estrogen plays a vital role beyond reproduction. It significantly influences brain function by supporting:- Synaptic plasticity and neurotransmitter balance
- Mitochondrial energy production
- Anti-inflammatory signaling
- Cerebral blood flow
The hippocampus and prefrontal cortex—regions responsible for memory and decision-making—are rich in estrogen receptors (Brinton, 2009). This makes them highly sensitive to hormonal fluctuations.
Estrogen Receptors and Their Role in the Brain
There are two primary types of estrogen receptors in the brain—ERα and ERβ. These receptors are located in areas critical for memory, mood regulation, and executive function. When estrogen binds to these receptors, it triggers molecular pathways that support neuronal health and brain plasticity (Bean et al., 2014).
During menopause, lower estrogen levels mean these receptors are no longer adequately stimulated, resulting in a disruption of these neuroprotective pathways.
How Starved Estrogen Receptors Contribute to Brain Fog
Starved estrogen receptors—those deprived of hormonal stimulation—fail to activate the mechanisms required for cognitive sharpness. This receptor deprivation may lead to:- Reduced synaptic strength and memory consolidation (Spencer et al., 2008)
- Mitochondrial dysfunction and oxidative stress (Brinton, 2008)
- Poor glucose metabolism in the brain (Mosconi et al., 2017)
- Increased neuroinflammation (Vegeto et al., 2006)
Scientific Evidence Linking Estrogen Loss to Cognitive Decline
Large-scale and imaging studies support the link between estrogen deprivation and brain changes:SWAN Study
Found that verbal memory and processing speed declined during the menopausal transition (Greendale et al., 2010)
PET Imaging
Mosconi et al. (2017) showed reduced glucose metabolism in postmenopausal women’s brains.
Animal Models
Show hippocampal shrinkage and cognitive decline with estrogen removal, reversible with supplementation (Frick, 2015)
Other Contributors to Brain Fog During Menopause
Although estrogen loss is central, other factors can amplify brain fog symptoms:
- Sleep disruption from night sweats and hot flashes (Freeman et al., 2015)
- Mood disorders due to serotonin imbalance (Sherwin, 2012)
- Suboptimal thyroid function (Chakrabarti & Pearce, 2013)
- Nutritional deficiencies like B12, iron, and omega-3s
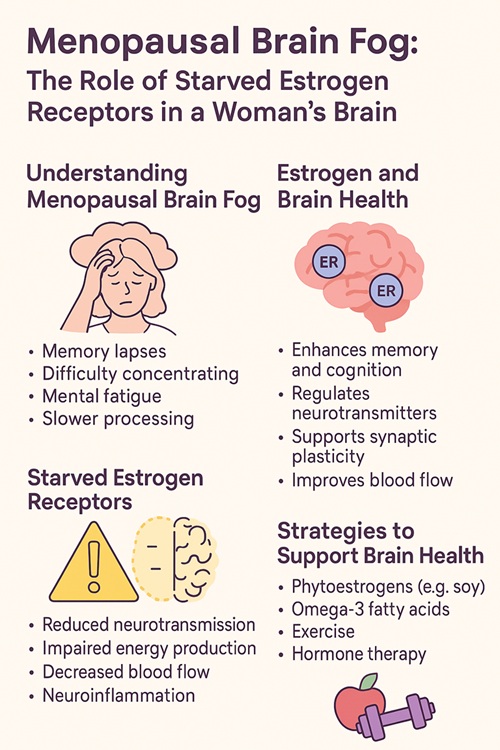
Natural Strategies to Improve Menopausal Brain Fog
Natural methods to support cognitive function during menopause include:
- Phytoestrogens: (from soy, flaxseed) mimic estrogen’s effects (Messina, 2014)
- Omega-3s: (EPA, DHA) support brain membrane function (Yurko-Mauro et al., 2015)
- B Vitamins: for neurotransmitter production (Smith & Refsum, 2016)
- Antioxidant-rich diet: berries, leafy greens, turmeric
- Regular aerobic exercise: increases brain-derived neurotrophic factor (Erickson et al., 2011)
- Mindfulness practices: help regulate stress (Goyal et al., 2014)
Emerging Treatments: Hormone Therapy and Alternatives
Hormone Replacement Therapy (HRT)HRT can relieve vasomotor symptoms and may support cognition—especially when started near the onset of menopause (early intervention theory). Estrogen therapy has shown:
- Improved verbal memory
- Reduced subjective brain fog
- Enhanced neural connectivity (Maki & Sundermann, 2009)
However, HRT is not without risks and must be individualized based on age, time since menopause, personal history, and preferences (North American Menopause Society, 2017).
Non-Hormonal Therapies
Selective Estrogen Receptor Modulators (SERMs)SERMs act on estrogen receptors with tissue selectivity, providing estrogen-like benefits in the brain while avoiding stimulation in the breast and endometrium. Raloxifene, for instance, has shown promise in improving verbal memory and executive function in postmenopausal women (Yaffe et al., 2001; Maki et al., 2009).
Neuroprotective SupplementsSeveral natural compounds are under investigation for their ability to support cognitive function during menopause:
Bacopa monnieri improves attention, memory recall, and processing speed (Calabrese et al., 2008).
Curcumin, the active component of turmeric, demonstrates anti-inflammatory and antioxidant properties that may protect against cognitive decline (Small et al., 2018).
Phosphatidylserine, a phospholipid component of neuronal membranes, has been shown to support working memory and reduce cortisol-related cognitive impairment (Vakhapova et al., 2010).
Ginkgo biloba extract has been studied for improving cognitive function in aging populations and may offer modest benefit, especially in early stages of cognitive decline (Gauthier & Schlaefke, 2014).
As with every other article, if you are considering taking on a nutritional or herbal supplement, first consult with a Clinical Dietitian - Nutritionist or a Naturopath or a Pharmacist or a Functional GP. Over supplementation or wrong supplementation or interaction between a supplementation and medication can lead to kidney or liver failure or even heart issues.
Be cautious, consult with a health professional first.
Cognitive TrainingCognitive training programs, particularly those involving computer-based tasks, have demonstrated efficacy in improving executive function, working memory, and processing speed in postmenopausal women (Lampit et al., 2014). These effects may be amplified when paired with physical exercise, which enhances neuroplasticity and blood flow to the brain (Ngandu et al., 2015).
Conclusion
Menopausal brain fog is a scientifically grounded phenomenon driven by hormonal changes—especially starved estrogen receptors in the brain. Understanding the neurobiology of menopause can empower women to take proactive steps to protect memory and focus. From natural supplements and exercise to hormone therapy and cognitive tools, solutions are available to help women regain mental clarity and thrive through menopause.
References
Bean, L. A., Ianov, L., & Foster, T. C. (2014). Estrogen receptors, the hippocampus, and memory. Neuroscientist, 20(5), 534–545. https://doi.org/10.1177/1073858413519865Brinton, R. D. (2008). The healthy cell bias of estrogen action: Mitochondrial bioenergetics and neurological implications. Trends in Neurosciences, 31(10), 529–537.
Brinton, R. D. (2009). Estrogen-induced plasticity from cells to circuits: Predictions for cognitive function. Trends in Pharmacological Sciences, 30(4), 212–222.
Calabrese, C., Gregory, W. L., Leo, M., Kraemer, D., Bone, K., & Oken, B. (2008). Effects of a standardized Bacopa monnieri extract on cognitive performance, anxiety, and depression in the elderly: A randomized, double-blind, placebo-controlled trial. Journal of Alternative and Complementary Medicine, 14(6), 707–713.
Frick, K. M. (2015). Molecular mechanisms underlying the memory-enhancing effects of estradiol. Hormones and Behavior, 74, 4–18.
Freeman, E. W., Sammel, M. D., & Gross, S. A. (2015). Sleep difficulties and cognitive performance during the menopause transition. Menopause, 22(9), 1005–1011.
Gauthier, S., & Schlaefke, S. (2014). Efficacy and tolerability of Ginkgo biloba extract EGb 761® in dementia: A systematic review and meta-analysis of randomized placebo-controlled trials. Clinical Interventions in Aging, 9, 2065–2077.
Gogos, A., Sbisa, A. M., Sun, J., Gibbons, A., Udawela, M., & Dean, B. (2014). A role for estrogen in schizophrenia: Clinical and preclinical findings. International Journal of Endocrinology, 2014, 1–16.
Greendale, G. A., Huang, M. H., Wight, R. G., Seeman, T., Luetters, C., Avis, N. E., ... & Karlamangla, A. S. (2010). Effects of the menopause transition and hormone use on cognitive performance in midlife women. Neurology, 72(21), 1850–1857.
Goyal, M., Singh, S., Sibinga, E. M. S., Gould, N. F., Rowland-Seymour, A., Sharma, R., ... & Haythornthwaite, J. A. (2014). Meditation programs for psychological stress and well-being. JAMA Internal Medicine, 174(3), 357–368.
Lampit, A., Hallock, H., & Valenzuela, M. (2014). Computerized cognitive training in cognitively healthy older adults: A systematic review and meta-analysis of effect modifiers. PLoS Medicine, 11(11), e1001756.
Maki, P. M., Rich, J. B., & Rosenbaum, R. S. (2009). Implicit memory varies as a function of estrogen replacement therapy in postmenopausal women. Neuropsychology, 23(5), 564–576.
Maki, P. M., & Henderson, V. W. (2012). Hormone therapy, dementia, and cognition: The Women’s Health Initiative 10 years on. Climacteric, 15(3), 256–262.
Maki, P. M., & Sundermann, E. (2009). Hormone therapy and cognitive function. Human Reproduction Update, 15(6), 667–681.
Messina, M. (2014). Soy foods, isoflavones, and the health of postmenopausal women. The American Journal of Clinical Nutrition, 100(Suppl 1), 423S–430S.
Mosconi, L., Rahman, A., Diaz, I., Wu, X., Scheyer, O., Hristov, H. W., ... & Brinton, R. D. (2017). Increased Alzheimer's risk during the menopause transition: A 3-year longitudinal brain imaging study. PLOS ONE, 12(12), e0185926.
Ngandu, T., Lehtisalo, J., Solomon, A., Levälahti, E., Ahtiluoto, S., Antikainen, R., ... & Kivipelto, M. (2015). A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): A randomised controlled trial. The Lancet, 385(9984), 2255–2263.
North American Menopause Society. (2017). The 2017 hormone therapy position statement. Menopause, 24(7), 728–753.
Ogiue-Ikeda, M., Tanabe, N., & Mukai, H. (2008). Estrogen and brain function: Role in neurotransmission and neuroprotection. Endocrine Journal, 55(3), 317–324.
Sherwin, B. B. (2012). Estrogen and cognitive functioning in women. Endocrine Reviews, 34(3), 345–355.
Small, G. W., Siddarth, P., Li, Z., Miller, K. J., Ercoli, L. M., Emerson, N. D., ... & Bookheimer, S. Y. (2018). Memory and brain amyloid and tau effects of a bioavailable form of curcumin in non-demented adults: A double-blind, placebo-controlled 18-month trial. The American Journal of Geriatric Psychiatry, 26(3), 266–277.
Smith, A. D., & Refsum, H. (2016). Homocysteine, B vitamins, and cognitive impairment. Annual Review of Nutrition, 36, 211–239.
Spencer, J. L., Waters, E. M., Romeo, R. D., Wood, G. E., Milner, T. A., & McEwen, B. S. (2008). Uncovering the mechanisms of estrogen effects on hippocampal function. Frontiers in Neuroendocrinology, 29(2), 219–237.
Vakhapova, V., Cohen, T., Richter, Y., Herzog, Y., & Korczyn, A. D. (2010). Phosphatidylserine containing omega-3 fatty acids may improve memory abilities in non-demented elderly with memory complaints: A double-blind placebo-controlled trial. Dementia and Geriatric Cognitive Disorders, 29(5), 467–474.
Vegeto, E., Benedusi, V., & Maggi, A. (2006). Estrogen anti-inflammatory activity in brain: A therapeutic opportunity for menopause and neurodegenerative diseases. Frontiers in Neuroendocrinology, 27(4), 477–484.
Yaffe, K., Krueger, K., Cummings, S. R., Blackwell, T., Henderson, V. W., & Sarkar, S. (2001). Effect of raloxifene on cognition and mood in postmenopausal women: A randomized controlled trial. JAMA, 285(16), 2129–2135.
Yurko-Mauro, K., McCarthy, D., Rom, D., Nelson, E. B., Ryan, A. S., Blackwell, A., ... & Stedman, M. (2015). Beneficial effects of docosahexaenoic acid on cognition in age-related cognitive decline. Alzheimer’s & Dementia, 6(6), 456–464.
Zhang, Q. G., Wang, R. M., Mahesh, V. B., & Brann, D. W. (2010). Estrogen and cerebral ischemia. Frontiers in Neuroendocrinology, 31(2), 105–118.
