Vitamin D: The Elixir of Life
Introduction
Vitamin D is not really a nutrient though it is treated as one, as in normal conditions, your skin on exposure to sun is able to supply your body with this. Also the active form of Vitamin D (1,25 dihydroxyvitamin D) is made by your kidney so it is more like a hormone.
Vitamin D helps to keep the calcium level in the blood by increasing the ability of the small intestine to absorb calcium from the diet. It also helps to absorb phosphorus from diet. Vitamin D thus helps your body to keep your bones, muscles strong.
Vitamin D has been shown to play a significant role with your immune system, your brain and also your nervous system.
Sources of Vitamin D
The sun is the best source of Vitamin D as Vitamin D is produced directly by the effect of the sun on the skin. If the skin has enough exposure to the sun, then the body will get sufficient vitamin D.
However, a limited amount of food also has vitamin D. These are:
- Fatty or oily fish like Salmon, Sardines, Mackeral
- liver
- Juice fortified with Vitamin D
- Certain spreads fortified with Vitamin D
- Dairy foods fortified with Vitamin D.
Vitamin D Deficiency Symptoms
In children, Vitamin D deficiency can lead to development of rickets (bowed and bent legs). In adults, this can lead to osteomalacia.
Other symptoms of Vitamin D deficiency are:
- muscle fatigue
- pain
-hair loss
- low mood
- impaired healing
- frequent infections or sickness.
Role of Vitamin D in Development of Diseases
Discovery of Vitamin D receptors on the immune cells have led to quite a lot of research on the role of Vitamin D deficiency has progression of certain illnesses.
1. Vitamin D and Respiratory Disease
Vitamin D was used more than 60 years ago for treatment of tuberculosis (before the advent of antibiotics. Low serum 25(OH)D are associated with higher risk of active tuberculosis (1).
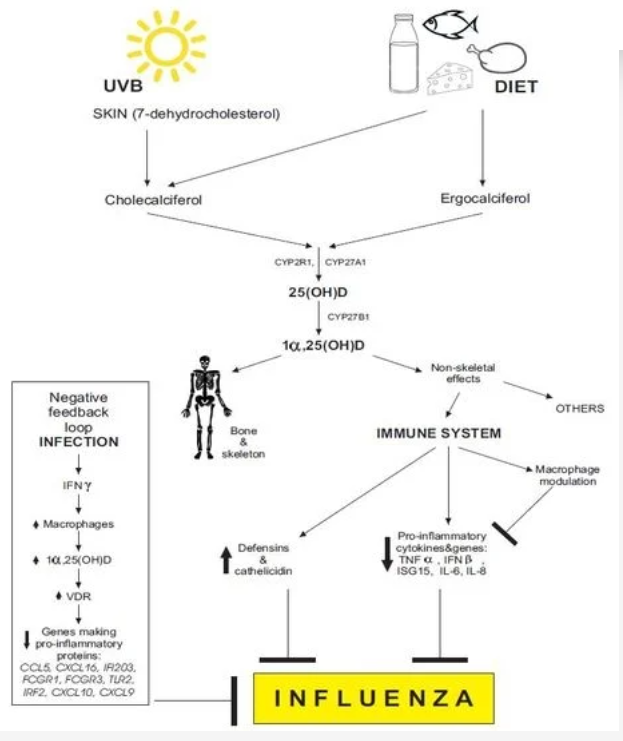
Lack of sun exposure in winter months leading to low serum vitamin D levels had been postulated to contribute to increased influenza in the winter months (2). The illustration below summarises how this could work (ref 2 - open source acknowledged):
A randomised double blind study to see the impact of vitamin D supplementation in school children to prevent Influenza A was undertaken in 2008 (3). Four hundred and thirty (430) children (aged 6 to 15 years old with mean age of 10.2 years old) were divided into a supplemented group (having 1200IU per day) or a placebo group. The study was taken from 1 November 2008 to 15 December 2008. 334 children were followed right through the study with 96% compliance to taking the tablets. There was a significant reduction in incidence of Influenza A in children taking Vitamin D supplement compared to those who did not (10.8% compared to 18.6% with relative risk of 0.58%) and also those children with previous history of asthma had lower incidence of asthma during this season.
2. Vitamin D and Covid 19
A systematic review by Yisak et al (2021) looked into the relationship between Covid 19 patients and Vitamin D status. Cell culture analysis shows that vitamin D specifically can act against enveloped virus and Covid 19 is an enveloped virus. With one of the causes of death for Covid 19 being serious acute respiratory syndrome with inflammation of the lungs and uncontrolled oxidative stress, the role of Vitamin D has been of interest in both infection, prognosis and treatment for Covid 19.
Of the 337 eligible papers from a comprehensive Pubmed and Google Scholar search, 9 papers were included in the final review. These had altogether 1,005,042 Covid 19 patients (participants).
Analysis of the data showed the following:
- increased level of hospitalization was associated with Vitamin D deficiency
- disease severity was associated with Vitamin D deficiency and
-ICU admission was higher in Vitamin D deficient individual.
Of note is a review by Danashkhah et al (5) on the role of vitamin D in suppressing cytokine storm in Covid 19 and associated mortality. They had data from countries that had more than 5000 confirmed Covid 19 cases. The biggest finding of this report was the potential of use of Vitamin D in reducing cytocine storm in patients with Covid 19. A cytokine storm is a uncontrolled immune response where the immune system produces a high level of proteins called cytokine. High levels of cytokines cause an overproduction of interleukin 6 and an exhaustion of lymphocytes. A high level of cytokines lead to epithelial and endothelial apoptosis (destruction), vascular leakage, acute respiratory distress syndrome and death (6).
Thus Danashkhah showed that treating Vitamin D deficiency reduced CRP levels (CRP is an infection marker and high level of this is an proxy marker for cytokine storm).
3. Vitamin D and Schizophrenia
It is thought that the development of schizophrenia has both genetic and environmental components. Of the environmental components, low serum vitamin D has been found in those with schizophrenia (7-9).
In the Yuksel et al study, 41 patients with remission in schizophrenia, 40 patients with acute schizophrenia and 40 patients with no psychopathology were recruited. They were tested for disease activity, total vitamin D (D2+D3), calcium, phosphate and parathyroid hormone levels. Demographics were collected for age, weight, daily sun exposure, nutrition, gender, skin colour and ethnicity.
Patients with acute schizophrenia had significantly lower Vitamin D levels than those in remission or with control (they were around two times lower). There was no difference between them for calcium, phosphate or parathyroid hormones.
A similar finding was noted by Crews et al (8) where they found that those with first episode psychosis were 2.99 more likely to be Vitamin D deficient compared to healthy controls.
Interestingly, the study by McGrath et al (9) of 9114 Finish subjects born in 1964 showed that the males that had Vitamin D supplementation in the first year of their lives has significantly less risk of developing schizophrenia by the age of 31 years old. There was no difference found within female subjects.
It is not known if Vitamin D deficiency is the cause of development of schizpphrenia.
A lab study was done of brains of neonatal rats (10) born of mothers deprived from vitamin D (either via exposure to sun or through diet). The study showed that vitamin D deficiency significantly changed the shape and size of the neonatal brain and altered the structure of the brain such as causing enlargement of ventricles and thinning of corticals (all of which is associated with schnizophrenia).
5. Vitamin D and Cancer
A 2018 review of vitamin D metabolism and function in cancer found that there was an inverse correlation between serum 25-hydroxyvitamin D (25(OH)D levels and high risk of colon, breast, prostate and other cancers (11). It also found that Vitamin D potentially had antitumorigenic effect.
This review states that vitamin D plays a key role in preventing the initiation stage of cancer by providing an anti-oxidant and anti-inflammatory defence and helping with repairing of damaged DNA through multiple complex signalling pathways.
Once the tumor has been initiated, vitamin D then acts by blocking the tumor cells from multiplying and helping the cells to self-destruct by switching the cells from wanting to survive to causing it to die. However, it looks as if the cancer cells also fight back Vitamin D’s interference by reducing the amount of vitamin D receptors it has on its surface. Therefore the fight is on for survival by cancer cells.
6. Vitamin D and Pre-Diabetes
Pre-diabetes is a condition where the blood sugar level is higher than normal range but not high enough to be labelled Diabetes Type 2.
Low serum 24-hydroxyvitamin D (25(OH)D) has been associated with impaired glucose intolerance (12).
A four year community based study in China tracking vitamin D levels and incidence of pre-diabetes or diabetes type 2 showed that low serum levels of 25(OH)D were an independent predictor of pre-diabetes or T2DM (13). In this study, from the initial 856 participants that were considered (aged between 20-74 years old), only 490 made it to the final analysis. Others were excluded due to death or lost during follow up or because of liver dysfunction, renal dysfunction, cancer, severe GI disorders or those taking vitamin D supplements. The 490 participants were free from pre-diabetes or type 2 diabetes at baseline. They had their glucose, insulin and 25 (OH)D levels measured at the start of the study and then 4 years later. Of these 48.5% developed prediabetes and 15.8% developed Type 2 Diabetes. Of note is that those with low 25 (OH)D status were 3.01 times more likely to develop pre-diabetes and 5.61 times more likely to develop diabetes type 2.
In another study where 86 participants who had pre-diabetes and vitamin D deficiency were put into a double blind, placebo controlled randomised trial where 44 of them received Vitamin D3 and 39 were in the control group (14). After 6 months, those in the dosed group bad significantly higher 25 hydroxyvitamin D levels than the control group. The insulin resistance in the supplemented group was significantly lower than the non-supplemented group ((HOMA-IR score of 2.6 to 3.1). The rate of progression to diabetes was significantly lower in the supplemented group compared to the non-supplemented group (where only 3% developed Type 2 diabetes in the supplemented group compared to 28% in the non-supplemented group.
This finding is echoed by the metanalysis of three (3) large trials that reported between 10% to 13% reduction in the development of diabetes type 2 in persons supplemented with vitamin D when compared to the placebo group (14).
7. Other Medical Conditions
There are other medical conditions where vitamin D deficiency especially severe deficiency may be a causal factor and appropriate supplementation likely help with the management of these conditions. These include include depression (15,16), fertility (17-19), dementia and Alzheimers (20).
Vitamin D Toxicity
Vitamin D is a fat soluble Vitamin so there are concerns of excessive supplementation.
Early symptoms of Vitamin D toxicity include (21):
- GI disorders like diarrhoea, anorexia, constipation, nausea and vomitting.
- bone pain,
- drowiness
- continuous headaches,
- irregular heartbeat
- joint pain
- muscle pain
- loss of appetite
- weakness
- nervousness
- twitching
- kidney stones.
Excessive supplementation can also cause hypercalcemia.
References
1. Nnoaham K, Clarke A Low serum Vitamin D levels and tuberculosis: a systematic review and meta-analysis. International Journal of Epidermiology (2008:37(1): 113-9)
2. Beata M, Griner-Bzura: Vitamin D and influenza - prevention or therapy. International Journal of Molecular Medicine (2018) 19(8): https://www.mdpi.com/1422-0067/19/8/2419
3. Urashima M et al. Randomized trial of vitamin D supplementation to prevent seasonal influenza A in school children. Amercan J Clin Nutr (2010):91 (5) 1255-1260 https://doi.org/10.3945/ajcn.2009.29024).
4. Yisak et al. Effects of Vitamin D on Covid-19 infection and prognosis: a systematic review. Risk Management and Health Care Policy (2021): 14(31-38) https://dopi.org/10/2147/RMHP.S2915845.
5. Daneshkhah A et al. Evidence of possible association of Vitamin D status with cytokine storm and unregulated inflammation in Covid-19 patients. Ageing Clin Exp Res (2020)32(10)1214-2158 https://pubmed.ncbi.nlm.nih.gov/32876941/
6. Tang Y et al. Cytokine storm in Covid-19. The current evidence and treatment strategies. Frontiers in Immunology 2020 (11)1708: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7365923
7. Yuksel R et al. Correlation between total vitamin D levels with psychotic psychopathology in patients with schizophrenia: therapeutic implications for add-on vitamin D augmentation. Ther Adv Psychopharmacol (2014):4(6) 268-275 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4257987/
8. Crews M et Vitamin D deficiency in the first episode psychosis: a case-control study. Schizophr Res 2013: 150: 533-537. https://pubmed.ncbi.nlm,nih.gov/24060571
9. McGrath J et al. Vitamin D supplementation during the first year of life and risk of schizophrenia: a Finnish birth cohort study. Schizophr Res 2004 Apr 1;67(2-3):237-45. https://pubmed.ncbi.nlm.nih.gov/14984883
10. Eyles et al. Vitamin D3 and brain development. Neuroscience (2003) 118(3): 641-53 https://pubmed.ncbi.nlm.nih.gov/12710973/
11. Jeon S-M, Shin E-A. Exploring vitamin D metabolism and function in cancer. Exp Mol Med 2018 (50)4:20 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5938036/
12. Teegarden D, Donkin SS Vitamin D: emerging new roles in insulin sensitivity. Nutr Res Rev 2009: 22: 82-92 https://pubmed.ncbi.nlm.nih.gov/19555519/
13. Goa Y et al. Vitamin D and incidence of Pre-Diabetes or Type 2 Diabetes: a Four-Year Follow-Up Community Based Study. Hindawi Research Article/Open Access. Vol 2018 https://www.hindawi.com/journals/dm/2018/1926308
14. Anastassios GP et al. Vitamin D supplementation for prevention of type 2 Diabetes Mellites: to D or not to D? J Clin Endocrinol Metab (2020)105(12): 3721-3733 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7571449
15. Parker GB, Brotchie H, Graham RK. Vitamin D and depression. J Affec Disord 2017 (15) 208:56-61 https://pubmed.ncbi.nlm.nih.gov/27750060/
16. Anglin RES et al. Vitamin D deficiency and depression in adults: systematic review and meta-analysis. Br J Psychiatry (2013) 202:100-7 https://pubmed.ncbi.nlm.nih.gov/23377209/
17, Cito G et at. Vitamin D and Male Fertility: An Updated Review. World J Mens Health 2020 (38)2:164-177 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7076312/
18. Voulgaris N et al. Vitamin D and aspects of female fertility. Hormones (Athens) 2017(16)1:5-21. https://pubmed.ncbi.nlm.nih.gov/28500824/
19. Lerchbaum E, Obermayer-Pietsch B. Vitamin D and fertility: a systematic review. Eur J Endocrinol 2012(166)5:765-78 https://pubmed.ncbi.nlm.nih.gov/22275473/
20. Chai B et al. Vitamin D deficiency as a risk factor for dementia and Alzheimer’s disease: an updated meta-analysis. BMC Neurol 2019(19)284 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6854782
21. Schwalfenberg G. Not enough Vitamin D. Can Fam Physician (2007) 53(5):841-854 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1949171
A randomised double blind study to see the impact of vitamin D supplementation in school children to prevent Influenza A was undertaken in 2008 (3). Four hundred and thirty (430) children (aged 6 to 15 years old with mean age of 10.2 years old) were divided into a supplemented group (having 1200IU per day) or a placebo group. The study was taken from 1 November 2008 to 15 December 2008. 334 children were followed right through the study with 96% compliance to taking the tablets. There was a significant reduction in incidence of Influenza A in children taking Vitamin D supplement compared to those who did not (10.8% compared to 18.6% with relative risk of 0.58%) and also those children with previous history of asthma had lower incidence of asthma during this season.
2. Vitamin D and Covid 19
A systematic review by Yisak et al (2021) looked into the relationship between Covid 19 patients and Vitamin D status. Cell culture analysis shows that vitamin D specifically can act against enveloped virus and Covid 19 is an enveloped virus. With one of the causes of death for Covid 19 being serious acute respiratory syndrome with inflammation of the lungs and uncontrolled oxidative stress, the role of Vitamin D has been of interest in both infection, prognosis and treatment for Covid 19.
Of the 337 eligible papers from a comprehensive Pubmed and Google Scholar search, 9 papers were included in the final review. These had altogether 1,005,042 Covid 19 patients (participants).
Analysis of the data showed the following:
- increased level of hospitalization was associated with Vitamin D deficiency
- disease severity was associated with Vitamin D deficiency and
-ICU admission was higher in Vitamin D deficient individual.
Of note is a review by Danashkhah et al (5) on the role of vitamin D in suppressing cytokine storm in Covid 19 and associated mortality. They had data from countries that had more than 5000 confirmed Covid 19 cases. The biggest finding of this report was the potential of use of Vitamin D in reducing cytocine storm in patients with Covid 19. A cytokine storm is a uncontrolled immune response where the immune system produces a high level of proteins called cytokine. High levels of cytokines cause an overproduction of interleukin 6 and an exhaustion of lymphocytes. A high level of cytokines lead to epithelial and endothelial apoptosis (destruction), vascular leakage, acute respiratory distress syndrome and death (6).
Thus Danashkhah showed that treating Vitamin D deficiency reduced CRP levels (CRP is an infection marker and high level of this is an proxy marker for cytokine storm).
3. Vitamin D and Schizophrenia
It is thought that the development of schizophrenia has both genetic and environmental components. Of the environmental components, low serum vitamin D has been found in those with schizophrenia (7-9).
In the Yuksel et al study, 41 patients with remission in schizophrenia, 40 patients with acute schizophrenia and 40 patients with no psychopathology were recruited. They were tested for disease activity, total vitamin D (D2+D3), calcium, phosphate and parathyroid hormone levels. Demographics were collected for age, weight, daily sun exposure, nutrition, gender, skin colour and ethnicity.
Patients with acute schizophrenia had significantly lower Vitamin D levels than those in remission or with control (they were around two times lower). There was no difference between them for calcium, phosphate or parathyroid hormones.
A similar finding was noted by Crews et al (8) where they found that those with first episode psychosis were 2.99 more likely to be Vitamin D deficient compared to healthy controls.
Interestingly, the study by McGrath et al (9) of 9114 Finish subjects born in 1964 showed that the males that had Vitamin D supplementation in the first year of their lives has significantly less risk of developing schizophrenia by the age of 31 years old. There was no difference found within female subjects.
It is not known if Vitamin D deficiency is the cause of development of schizpphrenia.
A lab study was done of brains of neonatal rats (10) born of mothers deprived from vitamin D (either via exposure to sun or through diet). The study showed that vitamin D deficiency significantly changed the shape and size of the neonatal brain and altered the structure of the brain such as causing enlargement of ventricles and thinning of corticals (all of which is associated with schnizophrenia).
5. Vitamin D and Cancer
A 2018 review of vitamin D metabolism and function in cancer found that there was an inverse correlation between serum 25-hydroxyvitamin D (25(OH)D levels and high risk of colon, breast, prostate and other cancers (11). It also found that Vitamin D potentially had antitumorigenic effect.
This review states that vitamin D plays a key role in preventing the initiation stage of cancer by providing an anti-oxidant and anti-inflammatory defence and helping with repairing of damaged DNA through multiple complex signalling pathways.
Once the tumor has been initiated, vitamin D then acts by blocking the tumor cells from multiplying and helping the cells to self-destruct by switching the cells from wanting to survive to causing it to die. However, it looks as if the cancer cells also fight back Vitamin D’s interference by reducing the amount of vitamin D receptors it has on its surface. Therefore the fight is on for survival by cancer cells.
6. Vitamin D and Pre-Diabetes
Pre-diabetes is a condition where the blood sugar level is higher than normal range but not high enough to be labelled Diabetes Type 2.
Low serum 24-hydroxyvitamin D (25(OH)D) has been associated with impaired glucose intolerance (12).
A four year community based study in China tracking vitamin D levels and incidence of pre-diabetes or diabetes type 2 showed that low serum levels of 25(OH)D were an independent predictor of pre-diabetes or T2DM (13). In this study, from the initial 856 participants that were considered (aged between 20-74 years old), only 490 made it to the final analysis. Others were excluded due to death or lost during follow up or because of liver dysfunction, renal dysfunction, cancer, severe GI disorders or those taking vitamin D supplements. The 490 participants were free from pre-diabetes or type 2 diabetes at baseline. They had their glucose, insulin and 25 (OH)D levels measured at the start of the study and then 4 years later. Of these 48.5% developed prediabetes and 15.8% developed Type 2 Diabetes. Of note is that those with low 25 (OH)D status were 3.01 times more likely to develop pre-diabetes and 5.61 times more likely to develop diabetes type 2.
In another study where 86 participants who had pre-diabetes and vitamin D deficiency were put into a double blind, placebo controlled randomised trial where 44 of them received Vitamin D3 and 39 were in the control group (14). After 6 months, those in the dosed group bad significantly higher 25 hydroxyvitamin D levels than the control group. The insulin resistance in the supplemented group was significantly lower than the non-supplemented group ((HOMA-IR score of 2.6 to 3.1). The rate of progression to diabetes was significantly lower in the supplemented group compared to the non-supplemented group (where only 3% developed Type 2 diabetes in the supplemented group compared to 28% in the non-supplemented group.
This finding is echoed by the metanalysis of three (3) large trials that reported between 10% to 13% reduction in the development of diabetes type 2 in persons supplemented with vitamin D when compared to the placebo group (14).
7. Other Medical Conditions
There are other medical conditions where vitamin D deficiency especially severe deficiency may be a causal factor and appropriate supplementation likely help with the management of these conditions. These include include depression (15,16), fertility (17-19), dementia and Alzheimers (20).
Vitamin D Toxicity
Vitamin D is a fat soluble Vitamin so there are concerns of excessive supplementation.
Early symptoms of Vitamin D toxicity include (21):
- GI disorders like diarrhoea, anorexia, constipation, nausea and vomitting.
- bone pain,
- drowiness
- continuous headaches,
- irregular heartbeat
- joint pain
- muscle pain
- loss of appetite
- weakness
- nervousness
- twitching
- kidney stones.
Excessive supplementation can also cause hypercalcemia.
References
1. Nnoaham K, Clarke A Low serum Vitamin D levels and tuberculosis: a systematic review and meta-analysis. International Journal of Epidermiology (2008:37(1): 113-9)
2. Beata M, Griner-Bzura: Vitamin D and influenza - prevention or therapy. International Journal of Molecular Medicine (2018) 19(8): https://www.mdpi.com/1422-0067/19/8/2419
3. Urashima M et al. Randomized trial of vitamin D supplementation to prevent seasonal influenza A in school children. Amercan J Clin Nutr (2010):91 (5) 1255-1260 https://doi.org/10.3945/ajcn.2009.29024).
4. Yisak et al. Effects of Vitamin D on Covid-19 infection and prognosis: a systematic review. Risk Management and Health Care Policy (2021): 14(31-38) https://dopi.org/10/2147/RMHP.S2915845.
5. Daneshkhah A et al. Evidence of possible association of Vitamin D status with cytokine storm and unregulated inflammation in Covid-19 patients. Ageing Clin Exp Res (2020)32(10)1214-2158 https://pubmed.ncbi.nlm.nih.gov/32876941/
6. Tang Y et al. Cytokine storm in Covid-19. The current evidence and treatment strategies. Frontiers in Immunology 2020 (11)1708: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7365923
7. Yuksel R et al. Correlation between total vitamin D levels with psychotic psychopathology in patients with schizophrenia: therapeutic implications for add-on vitamin D augmentation. Ther Adv Psychopharmacol (2014):4(6) 268-275 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4257987/
8. Crews M et Vitamin D deficiency in the first episode psychosis: a case-control study. Schizophr Res 2013: 150: 533-537. https://pubmed.ncbi.nlm,nih.gov/24060571
9. McGrath J et al. Vitamin D supplementation during the first year of life and risk of schizophrenia: a Finnish birth cohort study. Schizophr Res 2004 Apr 1;67(2-3):237-45. https://pubmed.ncbi.nlm.nih.gov/14984883
10. Eyles et al. Vitamin D3 and brain development. Neuroscience (2003) 118(3): 641-53 https://pubmed.ncbi.nlm.nih.gov/12710973/
11. Jeon S-M, Shin E-A. Exploring vitamin D metabolism and function in cancer. Exp Mol Med 2018 (50)4:20 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5938036/
12. Teegarden D, Donkin SS Vitamin D: emerging new roles in insulin sensitivity. Nutr Res Rev 2009: 22: 82-92 https://pubmed.ncbi.nlm.nih.gov/19555519/
13. Goa Y et al. Vitamin D and incidence of Pre-Diabetes or Type 2 Diabetes: a Four-Year Follow-Up Community Based Study. Hindawi Research Article/Open Access. Vol 2018 https://www.hindawi.com/journals/dm/2018/1926308
14. Anastassios GP et al. Vitamin D supplementation for prevention of type 2 Diabetes Mellites: to D or not to D? J Clin Endocrinol Metab (2020)105(12): 3721-3733 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7571449
15. Parker GB, Brotchie H, Graham RK. Vitamin D and depression. J Affec Disord 2017 (15) 208:56-61 https://pubmed.ncbi.nlm.nih.gov/27750060/
16. Anglin RES et al. Vitamin D deficiency and depression in adults: systematic review and meta-analysis. Br J Psychiatry (2013) 202:100-7 https://pubmed.ncbi.nlm.nih.gov/23377209/
17, Cito G et at. Vitamin D and Male Fertility: An Updated Review. World J Mens Health 2020 (38)2:164-177 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7076312/
18. Voulgaris N et al. Vitamin D and aspects of female fertility. Hormones (Athens) 2017(16)1:5-21. https://pubmed.ncbi.nlm.nih.gov/28500824/
19. Lerchbaum E, Obermayer-Pietsch B. Vitamin D and fertility: a systematic review. Eur J Endocrinol 2012(166)5:765-78 https://pubmed.ncbi.nlm.nih.gov/22275473/
20. Chai B et al. Vitamin D deficiency as a risk factor for dementia and Alzheimer’s disease: an updated meta-analysis. BMC Neurol 2019(19)284 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6854782
21. Schwalfenberg G. Not enough Vitamin D. Can Fam Physician (2007) 53(5):841-854 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1949171
