THAT GUT FEELING: GUT MICROBIOME AND HEALTH
Does your health depend on what bugs grow in your gut? The answer is yes! One hundred trillion bacteria, viruses, fungi, bacteriophage etc live in your gut and what they do can affect your health.
In the last decade,
one part of the human body is becoming a fore-runner to how the rest of the
human body functions. We are made of 1.1:1 Microbiome to Human
Cells1.
DNA Testing of Poos To
Greater Understanding Of Human Microbiome
For a long time, the use of culture mediums (those round dishes filled with special gels that had the growth solution for the bugs) were the primary means to identify gut bacteria and fungi.
These mediums have nutrients, growth promoting factors, energy sources, metals and buffers.
However, in order to grow what was in your gut, the labs had to have the right culture gels/mediums so that those bugs/fungi could grow in them,3.
That means the specialist / GP has to know what they suspect the bacteria is and then ask for the tests to be done for these.
Also, the amount of the poo has to be the right amount to give meaningful culture. So culture testing is limited.
With the development of DNA sequencing in the last 30 years, stool now can be tested for a whole range of microbiome species: bacteria, fungi, viruses and unculturable microorganisms.
The lab does not have to go through the process of growing the bacteria to try to identify them.
Scientists can now track how the gut microbiome changes through out life by DNA sequencing. The DNA sequencing test of microbes in a given sample is compared against the database of all the microbes they have already done the DNA sequence with. Hence the range of microbes is classified.
Introduction To “Commensal Microbiota”
A commensal is an organism that uses food supplied by the internal or external environment of the host, without establishing close association with it, for example, by feeding on its tissues4.
Known as “commensal microbiota”, the microbiome that live mostly in the intestine but also on skin, mouth and urinary tract, are made of bacteria, bacteriophage, fungi, protozoa and viruses; many species and strains of these we did not know existence of except for DNA sequencing.
It is a symbiotic relationship5. A symbiotic relationship is one that benefits those involved. The Microbiota (around 1014 varieties5, of which only about 5000 species has been identified so far) helps digest what the human consumes, produces products that are taken by the human for metabolism, hormonal, immune and brain function and helps keep the human either healthy or on pathway to disease.
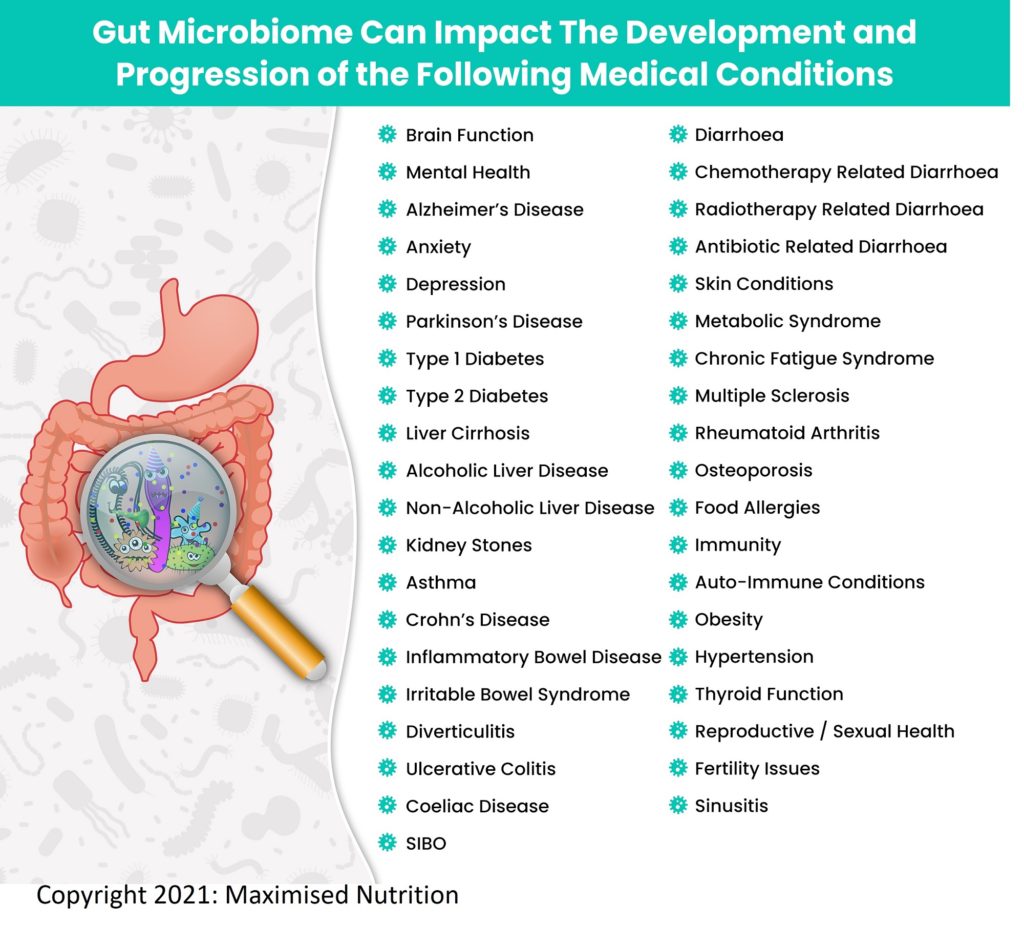
Medical Conditions
That Are Impacted By Gut Microbiome
The first lot of microbiota is introduced to a sterile baby coming out of the birth canal where she/he is introduced to the microbiota the mum carries6. The baby gets more exposure through breast milk and then with the first foods. There is a difference in gut microbiome of the baby born through birth canal and those both caesarean. Science now believes that these first microbiome provide the foundation for later health of that child, affecting the development of the digestive system, immunity and cognitive function. There may be other pathways where this first 1000 days of a baby impacts the microbiota and future health.
Using the DNA sequencing methodology, scientists have now identified the range of diseases/medical conditions influenced by the gut microbiota7-38 (see table below).
References
1. Sender Rm Fuchs S,
Milo R: Revised estimates for the number of human and bacteria cells in the
body. https://www.biorxiv.org/content/10.1101/036103v1
2. Sandle Tim, Assessment of Culture Media in Pharmaceutical Microbiology. American Pharmaceutical Review (2014) June 18 https://www.americanpharmaceuticalreview.com/Featured-Articles/163589-Assessment-of-Culture-Media-in-Pharmaceutical-Microbiology/
3. Identifying bacterial through look, growth, stain and strain. American Society for Microbiology. https://asm.org/Articles/2020/February/Identifying-Bacteria-Through-Look,-Growth,-Stain
4. Commensalism: Encyclopedia of Biodiversity (2001): 463-484 https://www.sciencedirect.com/science/article/pii/B0122268652002170
5. Eloe-Fadrosh EA, Rasko DA. The human microbiome: from symbiosis to pathogenesis. Annu Rev Med (2013): 64: 145-163 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3731629/
6. Young I. The infant microbiome: implications for infant health and neurocognitive function. Nurs Res (2016) Jan-Feb 65(1): 76-88 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4681407/
7. Eloe-Fadrosh EA, Rasko DA. The human microbiome: from symbiosis to pathogenesis. Annu Rev Med (2013): 64: 145-163 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3731629/
8. Pasolli E et al. Extensive Unexplored Human Microbiome Diversity Revealed by Over 150,000 Genomes from Metagenomes Spanning Age, Geography, and Lifestyle. Cell: Volume 176, Issue 3, 24 January 2019, Pages 649-662.e20
9. Mohajeri et al. Relationship between gut microbiome and brain function. Nutrition Reviews Vol 76, Issue 7, July 2018 pages 481-496
10. Vogt NM et al. Gut microbiome alterations in Alzheimer’s disease. https://www.nature.com/articles/s41598-017-13601-y
11. Yang B et al. Effect of regulating intestinal microbiota on anxiety symptoms: a systematic review. Gen Psychiatr 2019: 32(2) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6551444/#:~:text=Anxiety%20symptoms%20are%20common%20in,microbiota%20was%20related%20to%20anxiety.
12. Limbana T et al. Gut microbiome and depression: how microbes affect the way we think. Cureus (2020) 12(8) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7510518/#:~:text=By%20modulating%20gut%20microbiome%20composition,mood%20disorders%20develop%20%5B20%5D
13. Romano S et al. Meta-analysis of the Parkinson’s Disease gut microbiome suggests alternations linked to intestinal inflammation. https://www.nature.com/articles/s41531-021-00156-z#:~:text=The%20gut%20microbiota%20is%20emerging,nervous%20system%20accompany%20the%20disease.
14. Pheng P et al Gut microbiome in type 1 diabetes: A comprehensive review. Diabetes Metab Res Rev. 2018 Oct; 34(7): e3043. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6220847/#:~:text=Evidence%20so%20far%20has%20demonstrated,dominant%20in%20the%20faecal%20samples.
15. Gurang M et al. The role of gut microbiota in type 2 pathophysiology. https://www.thelancet.com/journals/ebiom/article/PIIS2352-3964(19)30800-X/fulltext
16. Tilg H et al. Gut microbiome and liver diseases. Gut 2016;65:2035–2044
17. Remazani A, Dominic SR The Gut Microbiome, Kidney Disease, and Targeted Interventions JASN April 2014, 25 (4) 657-670. https://jasn.asnjournals.org/content/25/4/657#:~:text=Alterations%20in%20gut%20microbiota%20and,%2C%20immune%20dysregaulation%2C%20and%20atheroscleroisis.
18. Baker P, Love D, Ferguson L Role of gut microbiota in Crohn's disease. Expert Rev Gastroenterol Hepatol (2009) Oct;3(5):535-46. https://pubmed.ncbi.nlm.nih.gov/19817674/
19. Zuo T, Ng SC, The gut microbiota in the pathogenesis and therapeutics of inflammatory bowel disease. Front Microbiol. 2018; 9: 2247 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6167487/
20. Andrei M et al. Intestinal microbiome, small intestinal bacterial overgrowth and inflammatory bowel diseases – what are the connections? Curr Health Sci J (2015): July-Sept, 41(3): 197-203 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6246988/
21. Fei Z et al. Gut microbiome associated with chemotherapy-induced diarrhea from the CapeOx regimen as adjuvant chemotheraphy in resected stage III colorectal cancer. Gut Pathogens (2019) 18 https://gutpathogens.biomedcentral.com/articles/10.1186/s13099-019-0299-4#:~:text=Diarrhea%20and%20gut%20microbiome%20disorders,lead%20to%20diarrhea%20%5B20%5D.
22. Zhung X et al. Fecal microbiota alterations associated with diarrhea-predominant irritable bowel syndrome. Microbiol (2018) 25 July https://www.frontiersin.org/articles/10.3389/fmicb.2018.01600/full
23. Chaysavanh M et al. The gut microbiota predispose to the pathophysiology of acute postradiotherapy diarrhoea. Am J Gastroenterology (2008) 103: 1754-1761
24. Yoon MY, Yoon SS Disruption of the gut ecosystem by antibiotics. Yonsei Med J (2018): 59(1)4-12 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5725362/
25. Pressemier BD et al. Gut-Skin Axis: Current knowledge of the Interrelationship between microbial dysbiosis and skin conditions Microorganisms 2021, 9, 353. https://doi.org/10.3390/ microorganisms9020353
26. Wang Peng-Xu et al. Gut microbiota and metabolic syndrome. Chinese Medical Journal (2020) April 5: 133 (7): 808-816
27. Giloteaux L et al. Reduced diversity and altered composition of the gut microbiome in individuals with myalgic encephalomyelitis / chronic fatigue syndrome. Microbiome (2016): Article number 30 https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-016-0171-4
28. Amini ME et al. Gut microbiome and multiple sclerosis: new insights and perspective. International Immunopharmacology (2020) 88: 107024
29. Bodhe R, Balakrishnan B, Taneja V. The role of microbiome in rheumatoid arthritis treatment. Ther Adv Musculoskelet Dis (2019): 11 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6685117/
30. Ding K, Hua F, Ding Wenge. Gut microbiome and osteoporosis Aging Dis (2020):11(2): 438-447 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7069453/#:~:text=Gut%20microbes%20can%20increase%20bone,remains%20to%20be%20further%20proven.
31. Nance CL et al. The role of the microbiome in food allergy: a review. Children (Basel) (2020):7(6) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7346163/
32. Lee KH et al. The gut microbiota, environmental factors, and links to the development of food allergy. Clinical and Molecular Allergy (2020) https://clinicalmolecularallergy.biomedcentral.com/articles/10.1186/s12948-020-00120-x
33. Wu Hsin-Jung, Wu Eric. The role of gut microbiota in immune homeostasis and autoimmunity. Gut Microbes (2012) 3(1) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3337124/#:~:text=The%20gut%20microbiota%20that%20resides,dysregulation%2C%20leading%20to%20autoimmune%20disorders
34. Aoun A, Darwish F, Hamod N. The influence of the gut microbiome on obesity in adults and the role of probiotics, prebiotics and synbiotics for weight loss. Preventative Nutrition and Food Science (2020): 25(2):113-123 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7333005/#:~:text=It%20has%20been%20reported%20that,et%20al.%2C%202018).
35. Pedro AJ, Raj D. Gut microbiota in hypertension. Curr Opin Nephrol Hypertens (2015): 24 (5): 403-9 https://pubmed.ncbi.nlm.nih.gov/26125644/#:~:text=Recent%20findings%3A%20The%20abundance%20of,and%20Dahl%20salt%2Dsensitive%20rats.
36. Knezevic J et al. Thyroid-Gut Axis: How does the microbiota influence thyroid function? Nutrients (2020): 12(6): 1769 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7353203/#:~:text=Gut%20microbiota%20also%20influences%20the,altered%20levels%20of%20these%20minerals.
37. Baker JM et al. Estrogen-gut microbiome axis: Physiological and clinical implications. Maturitas (2017): 103: 45-53 https://www.maturitas.org/article/S0378-5122(17)30650-3/fulltext
38. Mahboobeh M et al. A comprehensive review of the nasal microbiome in chronic rhinosinusitis (CRS) Clin Exp Allergy (2016) 46 (1): 21-41